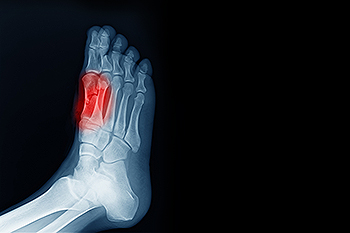
Understanding Heel Spurs
 Heel spurs are bony growths that develop on the underside of the heel bone, often causing pain and discomfort, especially when walking or standing for long periods. They typically form in response to strain on the muscles and ligaments of the foot. Heel spurs are commonly associated with conditions like plantar fasciitis or repetitive stress injuries. Factors such as obesity, wearing unsupportive shoes, and having high arches or flat feet can also contribute to the development of heel spurs. Symptoms may include sharp pain in the heel, especially during the first steps in the morning or after a long period of rest. There are numerous options when it comes to treating or preventing the formation of heel spurs. Rest, stretching exercises, orthotic inserts, injections, or surgery in more severe cases may be necessary. If you are experiencing symptoms of heel spurs, it is suggested you seek professional evaluation and treatment from a podiatrist to ensure your pain is alleviated and your health is protected.
Heel spurs are bony growths that develop on the underside of the heel bone, often causing pain and discomfort, especially when walking or standing for long periods. They typically form in response to strain on the muscles and ligaments of the foot. Heel spurs are commonly associated with conditions like plantar fasciitis or repetitive stress injuries. Factors such as obesity, wearing unsupportive shoes, and having high arches or flat feet can also contribute to the development of heel spurs. Symptoms may include sharp pain in the heel, especially during the first steps in the morning or after a long period of rest. There are numerous options when it comes to treating or preventing the formation of heel spurs. Rest, stretching exercises, orthotic inserts, injections, or surgery in more severe cases may be necessary. If you are experiencing symptoms of heel spurs, it is suggested you seek professional evaluation and treatment from a podiatrist to ensure your pain is alleviated and your health is protected.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact James Pak, DPM from California. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in Anaheim, CA . We offer the latest in diagnostic and treatment technology to meet your needs.
How to Treat Heel Spurs
Heel spurs are calcium deposits that cause bone protrusions on the heel bone. Heel spurs are usually associated with plantar fasciitis, which occurs when the plantar fasciitis in the foot becomes inflamed. Typically, heel spurs don’t cause any symptoms. However, they can produce chronic or intermittent heel pain. Those who have had the condition often describe the irritation as a stabbing pain.
There are risk factors that may make you more likely to develop heel spurs. People who have abnormal walking gaits, run and jog on hard surfaces, are obese, or wear poorly fitting shoes are more likely to develop heel spurs.
Fortunately, there are precautions you can take to avoid developing heel spurs. One of the best ways to do this is by wearing well-fitting shoes with shock-absorbent soles. Another preventative technique is to choose running shoes if you plan on running, and walking shoes if you plan on walking. Shoes are made for different activities and it is important to research a shoe before you purchase a pair.
The pain associated with heel spurs often decreases the more you walk. However, a recurrence of pain after an extended period of rest or walking is likely to occur with this condition. Those with severe heel spur pain may opt to go the surgical route for treatment. However, more than 90% of those with the condition get better without surgical treatment. If you have a heel spur and want to know if surgery is right for you, you should go to your podiatrist and he or she will be able to conduct a pre-surgical test or exam to determine if you are an optimal candidate for surgery.
Ankle Foot Orthoses
 An ankle-foot orthosis, or AFO, is a brace designed to support the ankle and foot, improving stability and alignment. It works by restricting movement in specific directions, thereby aiding in mobility and reducing the risk of injury. AFOs are commonly prescribed for individuals with conditions such as cerebral palsy, stroke, multiple sclerosis, or severe ankle arthritis. They are also used for drop foot, where the individual has difficulty lifting the front part of the foot. Diagnosing the need for an AFO involves a thorough examination by a podiatrist, including medical history, physical assessment, and sometimes imaging studies to understand the underlying condition and its severity. There are various types of AFOs, including rigid AFOs for maximum support, articulated AFOs allowing controlled movement, and dynamic AFOs designed for more natural movement. If you suffer from ankle pain, it is suggested that you schedule an appointment with a podiatrist for a diagnosis and treatment. If an AFO will help you, this foot doctor can provide personalized advice and a proper fitting.
An ankle-foot orthosis, or AFO, is a brace designed to support the ankle and foot, improving stability and alignment. It works by restricting movement in specific directions, thereby aiding in mobility and reducing the risk of injury. AFOs are commonly prescribed for individuals with conditions such as cerebral palsy, stroke, multiple sclerosis, or severe ankle arthritis. They are also used for drop foot, where the individual has difficulty lifting the front part of the foot. Diagnosing the need for an AFO involves a thorough examination by a podiatrist, including medical history, physical assessment, and sometimes imaging studies to understand the underlying condition and its severity. There are various types of AFOs, including rigid AFOs for maximum support, articulated AFOs allowing controlled movement, and dynamic AFOs designed for more natural movement. If you suffer from ankle pain, it is suggested that you schedule an appointment with a podiatrist for a diagnosis and treatment. If an AFO will help you, this foot doctor can provide personalized advice and a proper fitting.
If you are having discomfort in your feet and would like to try orthotics, contact James Pak, DPM from California. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact our office located in Anaheim, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Ankle Foot Orthotics for Athletes
Ankle foot orthotics are shoe inserts that offer support to control the placement and movement of the ankle, correct deformities, and compensate for weakness. These inserts are used to stabilize the foot and ankle and provide toe clearance during the swing phase of gate.
Athletes often suffer foot problems because their feet are not being supported within the shoe. Ankle and foot orthotics are custom made inserts that alleviate stress on the foot. However custom orthotics should be prescribed by a podiatrist who specializes in customized footwear and orthotics design. These inserts are used by athletes for different reasons. Runners use orthotics to absorb shock at heel contact and to set up the forefoot for push-off. Basketball players wear them to control their forefeet while jumping and running.
The two main types of orthotics are over-the-counter orthotics and custom-made orthotics. To be eligible for custom orthotics, an examination of the foot and ankle will need to be completed. Afterward, both the foot and ankle will need to be casted and fitted for the proper orthotic. When the fitting process is complete, adjustments can be made to make sure everything fits perfectly.
Over the counter orthotics tend to be more popular than custom fit ones. Athletes who have less severe aches and pains in the foot, ankle or lower back area can use the over-the-counter version of orthotics. Unfortunately, over-the-counter orthotics tend to not work in treating severe injuries or ailments. Whenever you suspect you may need an ankle foot orthotic, you should consult with your podiatrist to determine which type of orthotic is right for you.
Sesamoiditis and Bone Pain in the Feet
Sesamoiditis, a condition caused by inflammation of the sesamoid bones located beneath the big toe joint, can pose significant discomfort and mobility challenges. These small, pea-sized bones play a vital role in weight-bearing and stabilizing the foot during activities like walking and running. When subjected to excessive pressure or repetitive stress, the sesamoid bones may become inflamed, leading to symptoms such as sharp or dull pain beneath the big toe joint, and swelling. Sesamoiditis typically manifests as a gradual onset of pain, worsening with activity and improving with rest. Activities that involve pushing off the toes, such as jumping or running, may worsen symptoms. Diagnosis of sesamoiditis involves a comprehensive evaluation by a podiatrist, including a physical examination and possibly imaging tests such as X-rays or MRI scans. If you have pain under the big toe, it is suggested that you contact a podiatrist who can provide you with effective treatment solutions.
Sesamoiditis is an unpleasant foot condition characterized by pain in the balls of the feet. If you think you’re struggling with sesamoiditis, contact James Pak, DPM of California. Our doctor will treat your condition thoroughly and effectively.
Sesamoiditis
Sesamoiditis is a condition of the foot that affects the ball of the foot. It is more common in younger people than it is in older people. It can also occur with people who have begun a new exercise program, since their bodies are adjusting to the new physical regimen. Pain may also be caused by the inflammation of tendons surrounding the bones. It is important to seek treatment in its early stages because if you ignore the pain, this condition can lead to more serious problems such as severe irritation and bone fractures.
Causes of Sesamoiditis
- Sudden increase in activity
- Increase in physically strenuous movement without a proper warm up or build up
- Foot structure: those who have smaller, bonier feet or those with a high arch may be more susceptible
Treatment for sesamoiditis is non-invasive and simple. Doctors may recommend a strict rest period where the patient forgoes most physical activity. This will help give the patient time to heal their feet through limited activity. For serious cases, it is best to speak with your doctor to determine a treatment option that will help your specific needs.
If you have any questions please feel free to contact our office located in Anaheim, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Sesamoiditis
Sesamoiditis is a condition in which the sesamoid bones in the forefoot become inflamed from physical activity. Sesamoid bones are bones that are not connected to other bones but are located in tendons or muscle. Two of these sesamoid bones are very small and located on the underside of the foot near the big toe. Athletes such as runners, baseball and football players, and dancers are likely to experience sesamoiditis. Those with high arched feet, flat feet, or runners who run on the ball of their foot are also prone to suffer from sesamoiditis.
Symptoms include pain or throbbing on the ball of the foot near the big toe. The pain generally starts with a mild throbbing but gradually builds up to shooting pain. Bruising, swelling, and redness are possible, but in most cases, these symptoms are not present. However, moving the big toe can result in pain and difficulty.
To conduct a diagnosis, the podiatrist will examine the ball of the foot and big toe. They will look for any outliers and check the movement of the toe. X-rays will be taken to rule out any other conditions and ensure that it is sesamoiditis.
Treatment for sesamoiditis is generally mild and includes rest, anti-inflammatory and pain medication, and ice treatments to deal with the swelling and pain. Orthotics may be needed with people who have flat or high arched feet to relieve pressure off the bones. In some cases the toe will be taped and immobilized to allow healing. The podiatrist may also decide to use a steroid injection to help with swelling as well. If you have sesamoiditis, you shouldn’t engage in any intensive activity, as it may inflame the area and worsen your pain. If the sesamoid bone has fractured, surgery may be required to remove the sesamoid bone.
If you are suffering from sesamoiditis or are experiencing symptoms similar to sesamoiditis, you should stop all physical activity that puts strain on the area. Furthermore you should see a podiatrist for a diagnosis to see if you have sesamoiditis.
Identification and Diagnosis of Flat Feet

Flat feet, or fallen arches, are a common condition where the arches on the inside of the feet are flattened, allowing the entire sole to touch the floor while standing. This can be identified through a simple test. Wet your feet and stand on a flat surface where your footprint will show. A complete imprint of the sole indicates flat feet. Causes range from inherited genetic traits to weakened muscles in the feet and ankles due to aging or injury. While flat feet themselves are not always problematic, they can lead to complications such as foot pain, alignment issues with the ankles and knees, and increased risk of injuries. Management options include wearing supportive shoes, custom orthotic devices, engaging in exercises that strengthen foot muscles, and reducing activities that put excessive strain on the feet. If you have flat feet and have foot pain or mobility issues that persist, it is suggested that you see a podiatrist for a thorough evaluation and tailored treatment plan.
Flatfoot is a condition many people suffer from. If you have flat feet, contact James Pak, DPM from California. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our office located in Anaheim, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What is Flexible Flat Foot?
Flatfoot is classified as having the entire sole of the foot in contact or near contact to the ground while standing. The disorder is also known as fallen arches, because those affected have no arch in their feet. Flexible flatfoot and rigid flatfoot are the two types of flatfoot.
A person has flexible flatfoot if when sitting or standing on their toes, they have an arch that disappears when they stand with the entire foot on the ground. Flexible flatfoot may also be called “pediatric flatfoot” because the condition first appears in childhood. It is common among infants because the arch does not develop until the age of 5 or 6 years. Rigid flatfoot is not as common in children as it is with adults. This type of flatfoot is developed due to the weakening of tibialis posterior muscle tendon, a major supporting structure of the foot arch. Development of this deformity is progressive and shows early signs of pain and swelling that begins at the inside arch of the foot and moves to the outside of the foot below the ankle. More severe cases can possibly lead to arthritis of the foot and ankle joints.
Although most cases of flatfoot involve people born with the condition, some less common causes are obesity, diabetes, pregnancy, and osteoporosis. In some cases, flatfoot may come with no symptoms at all and does not require any type of treatment. With other cases though, symptoms may include pain in the shin, knee, hips and lower back. If a person with flatfeet experiences such symptoms, a health care provider may suggest using orthotic devices or arch supports, which may reduce the pain. Wearing supportive shoes can also prove more comfortable with flatfeet and staying away from shoes with little support such as sandals. Other methods to relieve pain also include stretching the Achilles tendon properly and using proper form when doing any physical activity. In addition, losing weight can reduce the stress on your feet and reduce the pain.
How Diabetic Patients Should Care for Their Feet

For people who have diabetes, foot care is not just a matter of comfort, it is imperative for preventing serious complications. High blood sugar levels can lead to nerve damage and poor circulation, increasing the risk of foot problems. Diabetic patients should inspect their feet daily for cuts, blisters, or signs of infection, and keep them clean and moisturized to prevent dryness and cracking. Wearing properly fitted shoes and socks is essential to prevent friction and pressure points. Regular appointments with a podiatrist are so important for diabetic foot care. Podiatrists can conduct comprehensive foot exams, assess nerve function and blood flow, and provide guidance on proper footwear and foot hygiene. They can also address any issues promptly, reducing the risk of complications such as diabetic ulcers or infections. If you have diabetes, it is strongly suggested that you schedule regular appointments with a podiatrist to safeguard your well-being and maintain mobility and comfort for years to come.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact James Pak, DPM from California. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our office located in Anaheim, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.